A Virginia Health System Prepares for Its Virtual Nursing Rollout
Mary Washington Healthcare, headquartered in Fredericksburg, Va., and virtual care company Caregility announced last month the deployment of an in-patient virtual engagement solution as part of the health system’s upcoming virtual nursing program.
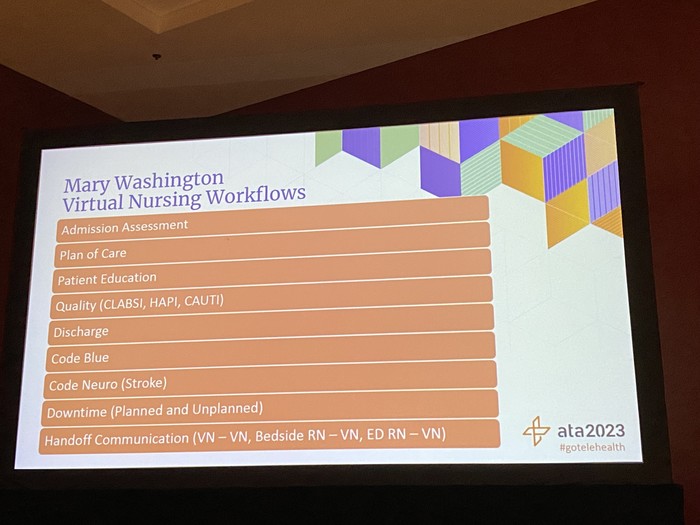
“It’s definitely exciting to be starting this new phase of care for our nursing staff and, of course, get safer outcomes for our patients,” Debra Marinari, associate vice president of hospital operations at Mary Washington Healthcare’s Stafford Hospital, said in her ATA2023 session.
Marinari did her research and proposed forging ahead with in-patient virtual support. In response, the two-hospital regional system turned to virtual nursing to mitigate the impact of a high nurse turnover rate, a lack of staff engagement and high labor costs.
The organization then tried a proof of concept for one nursing unit, using already-available Apple iPad devices from a previous initiative to save costs. At first, Marinari said, nurses were frustrated with workflows and buy-in was not there. But, as the proof of concept drew to a close, “toward the end, the nurses were like, ‘Wait a minute, where did all the virtual nurses go? We could use them,’ because they did see the benefits,” she said. The bedside nurses finally recognized that with a virtual nurse, they were free to focus on more immediate tasks and didn’t have to stay moored to discharge or admission.
Remembering her nurses’ initial frustrations, Marinari also decided to go with a solution to put cameras in patient rooms as a simpler measure for workflow purposes.