What makes a smart hospital so smart? You might think it’s the use of artificial intelligence and virtual care services, or strategic investments in IT infrastructure. Ultimately, however, the leaders at these healthcare organizations share one important trait: a commitment to technological innovation when it promises to positively affect patient care.
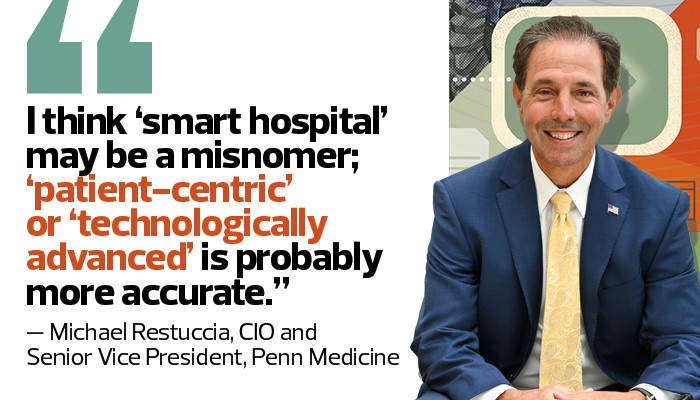
In a roundtable discussion, HealthTech heard from leaders at three healthcare systems that made Newsweek’s inaugural World’s Best Smart Hospitals 2021 list: from Penn Medicine in Philadelphia, Michael Restuccia, CIO and senior vice president, and John Donohue, vice president of entity services; from Rush University Medical Center in Chicago, acting Chief Medical Informatics Officer Dr. Jordan Dale; and from Hurley Medical Center in Flint, Mich., Dr. Michael Roebuck, chief medical information officer.
Click the banner below for access to exclusive HealthTech content and a customized experience.
HEALTHTECH: Tell us about the planning that goes into building a smart hospital. At what point did your organization decide to make technological innovation a goal?
RESTUCCIA: I think “smart hospital” may be a misnomer; “patient-centric” or “technologically advanced” is probably more accurate. Our perspective in the early design for our newest facility was, “How can we develop and build a hospital that can leverage technology to ensure the best care is delivered in the most effective and efficient manner?” Flexibility was a big part of that; having the cabling in place, for example, so that every room is both med-surg and ICU-ready.
DALE: It started about 12 years ago, when we decided to move to an electronic health record. That system is a source of so much rich data and has become foundational for how we’ve set up technology across the enterprise. The other big thing that set us up to be a smart hospital is network connectivity. We’ve prioritized having the bandwidth and high network reliability to really use mobile applications and other technologies for clinical decision-making, communication and patient monitoring.
ROEBUCK: With us, it was also our EHR. We went live with Epic in 2012, and that’s where I’d say we started our journey. Since then, we’ve had this constant push to maximize what we do in the technology space while always keeping our focus on patient care efficiency, quality and safety. We’re not a hospital that can spend money frivolously, so we’ve tried to make good choices about where we invest in technology.
HEALTHTECH: How has being a smart hospital helped during the pandemic?
DONOHUE: Our new facility was still in the construction phase, but we took a couple of floors that were further along and quickly brought in beds and enough monitoring gear to handle as many as 90 patients. We didn’t end up using it, but it was good to see we could easily flex in an emergency situation.
ROEBUCK: Our EHR helped us quickly standardize patient care with things such as order sets, best-practice alerts and decision support tools. Data visibility has been huge and was especially helpful for managing our census during the early waves — knowing who was where, what they had and how long they’d been here. We’ve really maximized telemedicine, and we’ve even had providers use it within the hospital to care for patients in other units. In our neonatal intensive care unit, they used telemedicine tools for remote rounding so everyone on the team could be there virtually without exposing babies to the risk of infection.
RELATED: Learn how interoperability increases efficiency and transparency in healthcare.
DALE: It’s allowed us to be innovative with clinical communication. Use of our secure texting platform in our EHR went up around 300 percent as providers tried to avoid face-to-face conversations and only used devices they knew were clean. COVID-19 has also proved we can stay ahead of the curve in managing capacity across our system. With predictive modeling and analytics, and using the data we have in our systems, we’re able to be proactive rather than reactive.
HEALTHTECH: Given your reliance on technology, how are you handling security?
DONOHUE: It’s front and center for us every day. With the Internet of Things and the medical IoT, every lightbulb in our new building is connected to the network, and all of our medical devices are connected, so security is always on our minds. The building is outfitted with network segmentation and access control, so we know what the profile is supposed to look like for every single device on-premises. We’re also focused on physical security with card swipes, hundreds of cameras. We’ve crossed all our t’s and dotted all our i’s.
DALE: We’ve been vigilant anytime we introduce anything new to our system and our network. My office is right across from our cybersecurity officer, and that’s for a reason. We can’t have our technology being at the bleeding edge and the security lagging behind.
ROEBUCK: Healthcare data is valuable. There are privacy laws we have to follow, and there are always users doing funny things to potentially expose your data. Security is an everyday, all-day priority, which is probably true for all hospitals.
HEALTHTECH: How are patients interacting with the implemented technologies? What’s next?
RESTUCCIA: We haven’t had patients in our new building yet, but the biggest thing they’ll notice in their rooms is the footwall monitor we call IRIS. It’s essentially a large-screen TV that gives them access to everything related to their care. They can use it to reach their clinical teams, to see their schedules, review their meds, order food and entertainment. They can use it for lighting and temperature control and for opening or closing their window shades. It’s all about patient engagement and being family-friendly, and operating in the most efficient and empathetic manner possible.
DALE: We’re a very progressive organization in terms of sharing notes and other clinical data with patients. They can bring their smartphones into the hospital and go into their MyChart accounts and see their vitals, their labs and everything else. It allows them to really be a part of their care.
Looking ahead, we’ll continue to develop our predictive modeling and analytics capabilities. We’ll also push our use of telemedicine, which right now, even without a COVID-19 surge, accounts for about 15 to 20 percent of our volume on the ambulatory side. We’re also pursuing voice technologies for our clinical staff.
READ MORE: Find out how natural language processing could be a game changer for EHR workflows.
ROEBUCK: Our patients really appreciate the connectivity. When I’m working in the emergency department, it’s often the case that they get lab values on their phones even before I see them. When they see their clinician barcode-scanning their medicine and confirming it’s the right drug, I think that gives them a sense of safety.
As far as future technologies, we’re always looking at ways to sift through the billions of data points that we generate and get the ones that are valuable in front of providers to affect patient care. Otherwise, our approach is always to explore things as we need them and as we see opportunities to do things better. That’s when we go out into the world of technology and look for the best solutions.