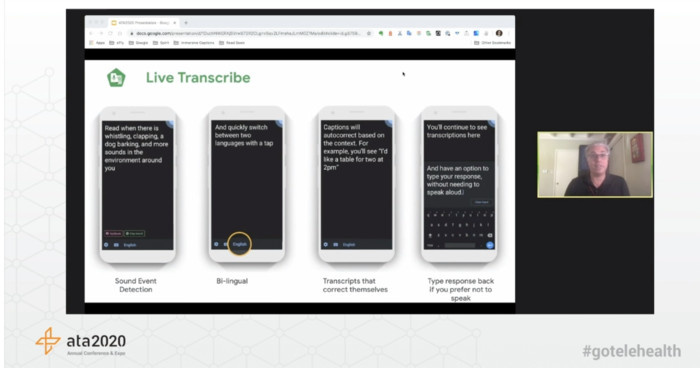
Transcription services will play a key role as telehealth services evolve, said Christopher Patnoe of Google.
Using creative thinking to adapt to their environment is a way of life for members of this population, she added, and the strategies can play an influential role in telehealth.
“Those are the kind of engineers people are looking to as we try to re-envision our world,” said Ellison, who has been paralyzed from the neck down since she was hit by a car in seventh grade, “not just out of charity but because we want to make people’s lives better, so they are active participants in society.”
READ MORE: The future of care delivery is here. Explore our complete coverage of telehealth and virtual care.
Addressing Social Determinants of Health to Improve Care Delivery
Prior to the pandemic, patients covered by Medicare and Medicaid couldn’t access telehealth without a number of restrictions. Medicare members, for example, once were limited by geography and applicable reasons for a visit. Medicaid is administered by states, which led telehealth coverage policies to vary widely.
Broader permanent coverage of telehealth services could be a game changer, making preventive care less of a barrier for patients who lack transportation, can’t secure childcare or who live in rural areas.
“We’re running into the same concerns as everyone else — fears around when these executive orders are going to end,” said Sydney Etheridge, director of the healthcare investment program at Planned Parenthood Federation of America.
Outreach remains critical as usage expands. Texas Children’s Hospital deployed television ads, social media and direct mail to promote the availability of telehealth, said Laura Laux Higgins, the hospital’s director for strategic projects. Staffers were trained with scripts to help assure parents new to the platform that virtual care is safe and effective.
Still, more work remains. Some health systems and insurers may go further to invest in the tools and get them in the hands of patients most in need.
“How can we have digital technology and not be prescribing Wi-Fi or not prescribe a smartphone?” said Grace Cordovano, a patient advocate and digital health consultant. “This is something that needs to become mainstream.”
Keep this page bookmarked for articles from the event. Follow us on Twitter @HealthTechMag as well as the official organization account, @AmericanTelemed, and join the conversation using the hashtags #ATA2020 and #GoTelehealth.