As digital health continues to expand capabilities and find further integration in traditional healthcare organizations, equity and access are major concerns for the industry.
Telehealth, for example, has been heralded as a great connector to care during a public health emergency. But broadband connectivity is still a barrier for millions of Americans, especially in rural areas. Digital literacy rates — knowledge and problem-solving in a tech-centered world, such as the ability to use an app store or two-factor authentication — point to stark divisions.
As healthcare organizations look to digital health tools to improve patient care, they need to be aware of the hurdles faced by the communities they serve. Industry experts at the ViVE 2022 conference shared their insights on achieving greater patient equity and access.
Click the banner below for access to exclusive HealthTech content and a customized experience.
Fitting Healthcare into Everyday Life
Dr. Jennifer Schneider, CEO of the recently launched, rural-focused health startup Homeward, shared her personal connection with rural communities, having grown up in one. As the former chief medical officer and president of the digital health company Livongo, she said she intends to apply lessons learned there to delivering hyperpersonalized care for rural communities.
“When you spend time in a community, there are community flows,” Schneider said, noting that places like churches, stores, barbershops and sports venues serve as community spaces. “It’s an identification and appreciation of what people in each unique location hold in esteem, where their daily flow is, and to meet them and be present or available to them.”
Moderator Nancy Brown (far right), General Partner at Oak HC/FT, introduces the “Addressing Inequitable Access #RuralHealthDilemma” session. Panelists, from right to left, included Anna Lindow, CEO and Co-Founder of Brave Health; Homeward’s Dr. Jennifer Schneider; Gil Addo, CEO and Co-Founder of RubiconMD; and Roshan Navagamuwa, Executive Vice President and CIO of CVS Health.
Whether it’s at home or during a Sunday afternoon grocery run, meeting patients where they are is key. “You’re trying to fit into the flow of people’s lives. You’re not asking people to step outside and do something that isn’t natural to them,” Schneider added.
MORE FROM VIVE: Find out 3 takeaways on the business of healthcare.
If It Isn’t Measured, It Doesn’t Matter
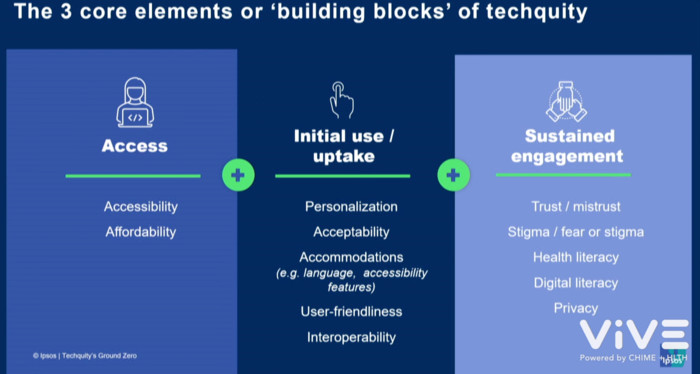
Before the industry panelists spoke about “techquity” — or technological equity — Alexis Anderson, principal at Ipsos, shared a presentation and a video capturing patient perspectives on tech access.
The patients featured in the video talked about their long work hours, poor internet access in their rural communities, inexperience with technology, wariness of sharing personal information through an online portal and reluctance to use smartphone apps because of privacy concerns.
Afterward, industry experts discussed the importance of trust and collecting key data so organizations can seriously commit to increasing equity and access.
Alexis Anderson, principal at Ipsos, shared a presentation ahead of the industry panel at the “Techquity’s Ground Zero” session.
Dr. Carlos M. Nunez, chief medical officer of medical device company ResMed, said that trust is discussed extensively within his company due to the enormous responsibility of protecting patient data.
“The word trust gets thrown around a lot inside of ResMed because we are asking a lot of patients. Their devices are being connected to the cloud and they are sending us a lot of data,” he said. “We’ve learned a lot about how data can be misused and how people can lose their privacy, their anonymity and their security online very easily.”
“Every conversation that we have in healthcare should be thinking about the equity component, just like we do with quality improvement,” said Dr. J. Nwando Olayiwola, chief health equity officer and SVP at Humana. “If it’s not on your scorecard, it’s probably not a priority for your organization.”
RELATED: Learn how AI helps healthcare organizations reduce avoidable patient harm.
Failures in Value-Based Care
What has hampered healthcare organizations’ move toward value-based care?
First is trust — again, a major component that providers must build within their communities.
“Trust, in my mind, is built by a series of promises kept. I would say in the communities we tried to service and target, often we’ve missed the mark. We’ve not been particularly successful at delivering consistent care over time in a way that’s respectful of those communities,” said Dr. Vindell Washington, CEO of digital health management company Onduo.
Moderator Dr. Yele Aluko (center) is Managing Director and Chief Medical Officer for EY Americas at EY. He introduced the panelists for the “They Can’t Get No Satisfaction: Rethinking Care for Disaffected Patients” session. On the far right is Onduo’s Dr. Vindell Washington, with SameSky Health Founder and CEO Abner Mason next to him. On the far left is Dr. Pooja Mittal, Medical Director of Health Equity at Health Net, with Hilary Hatch, Chief Clinical Officer at Phreesia next to her.
Next, personalization must expand. Patients do not identify as their diseases, Washington said, therefore care and insight need to be structured and delivered in a way that considers the whole person. Individual care plans are crucial, and this change needs to happen at scale.
“Most of what happens in between physician visits and between caregiver visits is invisible,” Washington said. “The provider has no insight between this visit and the one that happens three months from now. The ability to have insight provided, the ability to have that data come back that becomes actionable, is a missing component.”
READ MORE: Here's how to make value-based care a widespread reality in healthcare.
Define Results To Assess Healthcare Solutions
“The way that we’ve taken our partnerships is to shift from just providing the tools that are going to help them continue to do the services that they’re offering to a solution in a value-based orientation,” said Royal Tuthill, general manager of ambulatory and population health at digital patient engagement company Get Well.
From left to right: Moderator Tarun Kapoor, Senior Vice President and Chief Digital Transformation officer of Virtua Health, introduces panelists for the “An Evite to Better Health” session: Get Well’s Royal Tuthill; Melissa Sherry, Vice President of Social Care Integration at Unite Us; and Manav Sevak, Co-Founder and CEO of Memora Health.
He said that at the beginning of a partnership, Get Well creates an ROI scorecard and explores what services are being provided and where the gaps are, creating a value metric for each service. When providers offer fragmented services, patients have a harder time navigating the system to get the right care in time. Get Well helps with that navigation, such as determining the value of reducing days in the NICU, for example, based on a scorecard, then helping to design programs to drive outcomes that align with mission and financial metrics. Online dashboards are available to partners so they can look at ROI over time and use it to manage and optimize programs.
Keep this page bookmarked for our ongoing virtual coverage of ViVE 2022. Follow us on Twitter at @HealthTechMag and join the conversation at #ViVE2022.