Complementary Upgrades Help Hospitals Get the Most out of EHR Deployments
When MD Anderson Cancer Center’s IT team researched options to replace its homegrown electronic health records system, it learned that vendors recommend virtualizing the EHR application for ease of management and performance consistency. But the provider didn’t stop there.
“We decided if we were going to do it, we might as well get the benefits of virtualization for the entire clinical desktop,” says Chuck Suitor, associate vice president and CTO for the Houston organization, explaining that the organization deployed a VMware Horizon View virtual desktop infrastructure across 8,000 thin clients.
That choice — along with other upgrades and implementations to support the Epic EHR installation, including switching to all-flash storage and Intel servers running Linux — proved to be almost as beneficial as the EHR itself, says Suitor, who believes that hospitals embarking on similar journeys must focus on care outcomes and patient safety first and foremost.
“Rather than just keeping costs as low as possible, our goal was a quality implementation,” he says. “You’re paying enough for EHR software; don’t go cheap on the infrastructure. Get the best deal that you can, but implement the infrastructure that you need so that patients can get the entire value from the software.”
As hospitals around the country reap the benefits of modern EHRs, many are finding that improvements to the rest of the infrastructure can extend the reach of their new solutions and optimize overall operations.
SIGN UP: Get more news from the HealthTech newsletter in your inbox every two weeks!
MD Anderson Phases EHR Deployments
The most important infrastructure upgrades to support an EHR implementation, aside from the EHR itself, are those that provide staff with access to medical data anywhere, using the device of their choice, says Gregg Pessin, a research director in healthcare delivery at Gartner. That’s why, for instance, VDI and EHR projects are tied so closely to one another, he says.
Because MD Anderson’s EHR upgrade morphed into such a comprehensive project, Suitor’s team implemented the technology in phases but went live with everything on a single day, in March 2017.
First came the VDI project, for which it deployed both VMware and Citrix solutions, in accordance with enterprise licensing agreements, as well as Cisco UCS B240 M4 servers and Dell EMC XtremIO storage. Monitors and keyboards were equipped with built-in fingerprint and archiving e-readers to enable ID card tap-and-go login.
MD Anderson also purchased Code CR1400 barcode scanners, Topaz SigLite card scanners, Ergotron carts and Zebra portable barcode printers. Before the upgrade, Suitor’s team didn’t receive many performance complaints, but staff expressed frustration about operational limitations because they couldn’t take advantage of modern patient safety and convenience features. That changed after the upgrade.

For instance, barcode administration ensures that patients are being administered the right medications at the right time and dosage. “That helps prevent medication errors,” Suitor says. “That’s a major feature we didn’t have before.”
From research to go-live, the organization collaborated with Epic and CDW, the latter of which worked with vendors to resolve issues as they arose. For instance, when MD Anderson needed more barcode readers than were available in the U.S., CDW secured extra devices from China quickly enough to keep the project on schedule.
Most of the issues, however, had less to do with technology than with organizational change. The goal was for the upgrades to be so seamless that they simplified, rather than complicated, staff and clinician workflows.
“We wanted to make it so the technology was a nonevent,” Suitor says, “so the staff could focus on the change necessary to modernize the operations of the institution.”
Baptist Health Builds an EHR Foundation for the Future
Baptist Health has used Cerner’s EHR for more than 10 years, but originally, it was only for basic pharmacy, lab and nursing documentation, which CIO Steve Miller jokingly calls “EHR lite.”
The Montgomery, Ala.-based hospital had ambitious plans. It began a computerized physician order entry (CPOE) utilization to improve patient care and qualify to meet federal EHR regulations, but with weekly outages, staff could barely complete basic tasks.
The network would drop connectivity while nurses scanned patient wristbands. Nurses couldn’t even play online training videos for fear it would crash the network.
“That’s how bad it was from a stability standpoint,” says Mallary Myers, Baptist Health’s system vice president of operational improvement and innovation.
While stability and performance were the primary drivers behind the organization’s network infrastructure upgrade, leadership also recognized that such an installation was necessary to achieve its strategic plan — adding wireless technologies such as oximeters, IV pumps, alerting and Voice over IP.
“We wanted to do something that not only solved the short-term pain but really set a foundation for the future,” says Miller, who’s employed by Cerner but serves as Baptist Health’s CIO.

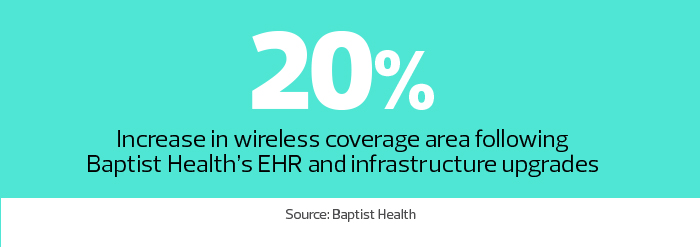
The organization selected Cisco for the 18-month, $7 million project, adding all new equipment in its facilities, including 300 Nexus and Catalyst switches, 120 wiring closets, 1,200 wireless access points and a new network with full redundancy in two data centers. It also laid new fiber optic and CAT 6e Ethernet cable.
Baptist Health went live with the new network in 2016. It has since added new wireless tools to the infrastructure, such as pulse oximetry, smartphones, patient monitors and secure messaging.
New technology, such as smart pump programming, infusion management, specimen collection and documentation in patient rooms with workstations on wheels, has made a profound difference in clinical workflows and patient safety. “You can’t do that if you don’t have a reliable infrastructure,” Myers says.
And instead of three to four minutes to log in to each device, it now takes a minute and a half the first login of the day, then a few seconds on each new device.
“When you think about going from four minutes every time you move from computer to computer to now 10 seconds — that has huge impact,” Miller says. “We don’t want the technology to get in the way of care. We want clinicians to focus on patients, not worry about the wireless network.”
Mount Sinai Taps a Strong IT Support System for EHR
Preparing infrastructure for an EHR rollout is always complex, but as Mount Sinai Health System’s Kristin Myers embarks on her fifth Epic hospital installation, she knows the drill.
Myers, senior vice president of IT at the New York organization, undertook her first Epic implementation in 2006. After the health system’s merger with Continuum Health Partners in 2013, she has steadily added to her list of projects, including two hospitals that went live this March. Next up is Mount Sinai Brooklyn, followed by a new hospital in downtown Manhattan and New York Eye and Ear Infirmary.
To achieve the benefits of EHRs — better care continuity, shortened hospital stays, reduced readmissions — the IT supporting the system must be stable and have near 100 percent uptime. “If you deploy an EHR on existing infrastructure, you are placing your transformation project at risk,” she says.
If a workstation loses connectivity with the wireless network, the physicians, nurses and other providers will become increasingly frustrated. “You need to make technology as efficient as possible for the physicians and nurses and not introduce barriers,” Myers says. “The adoption is impacted if the infrastructure is not completely stable and it doesn’t support the workflow.”
Roughly 15 percent of more than 900 IT employees at Mount Sinai are dedicated to Epic installations and support the optimization. The first thing they do when embarking on a new rollout is a complete walk-through of the hospital. They look at network closets, workstations, scanners, existing medication carts, emergency power and clinical equipment, such as vents and monitors. They test the wireless network to ensure that it’s ubiquitous.
The goal, Myers says, is for as much of the infrastructure as possible to meet Mount Sinai’s standards, which include Citrix to connect PCs to the EHR, Zebra barcode scanners and Samsung monitors for digital whiteboards.
“There are going to be areas that need to be customized for a particular workflow at each facility, but as a general rule, we try to standardize,” she says. “It’s really important because that’s how there is a standard of care that is consistent throughout the health system, where physicians can use the system at multiple hospitals, and from a technology perspective, you are able to leverage a centralized support model.”









