The panel for the “Reducing the Cost of Care With Data-Driven Care Management” digital session discussed the siloed nature of the U.S. healthcare system.
“We see a lot of unstructured data that’s out there. To what degree are they looking for new solutions to put some structure into that, to make it more usable or find ways of removing these data silos that exist within these organizations in order to make it more interoperable, for example?” To added.
Payers have the most data that goes unshared across the spectrum, Rocchio said, and stakeholders aren’t working together on a standardized data set.
“It’s not helping us across the continuum of care, but it’s siloing us on purpose,” she said. “We’re getting exactly what we designed.”
The fragmented data ecosystems within healthcare have produced what Anand called “the three Rs of efficiency.”
“We do a lot of redundant work — everybody does the same work. We do a lot of rework, because when everyone does the same work, they do it differently,” Anand said. “And then, when we’ve realized we’ve looked at it differently, we rework it. And then, even after we rework it, we don’t agree with each other, because you’ve got these siloed ecosystems. Then, we reconcile. And that’s how we spend all our money.”
MORE FROM HIMSS21: Anticipate the threat to enhance healthcare cybersecurity.
Why Interoperability Is Important to Healthcare Delivery
“Data is so important to the workflow of medicine,” said Dr. Mujeeb Basit, associate chief medical informatics officer and assistant professor at the UT Southwestern Medical Center in Dallas. “We’ve spent so much time creating complex solutions to solve downstream data problems, when in reality, we should be spending our time fixing the upstream data access.”
He highlighted the difficulties of creating quality metrics for every department in his organization and said improvements in institutionwide foundational systems are needed.
Healthcare organizations must design strategies to increase data liquidity and elevate meaningful information sharing among stakeholders seamlessly inside and outside of hospital walls, Basit added.
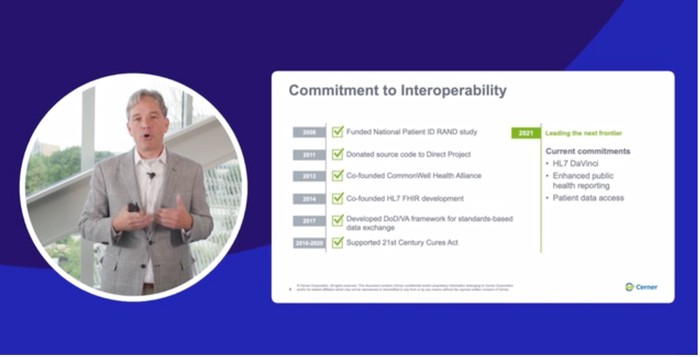
During a separate spotlight keynote session, Cerner President Donald Trigg spoke on the strategy behind excellent care delivery inside and outside the hospital.
Dynamic forces of change, accelerated by the COVID-19 pandemic, are rapidly reorganizing the healthcare industry and models of care delivery, Trigg said, so that leaders are focused on not only solving today’s challenges those of the next five years and beyond.