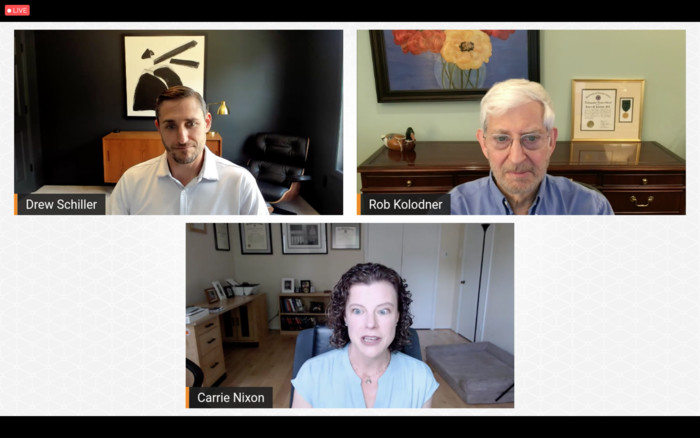
Remote Patient Monitoring Empowers Patients with Data
Physicians and patients often talk past each other, said Schiller, co-founder and CEO of Validic, a digital health platform that connects healthcare systems with remote patient data. For example, physicians may tell patients they need to exercise or follow a healthier diet, while patients say they’re trying but it’s not helping. RPM data can provide clarity and guide conversations with patients.
Validic partnered with Sutter Health in 2016 to capture patient data using RPM. One patient in the program with Type 2 diabetes had an A1C level consistently above 9 despite trying to manage his diet and walk regularly. Consistent tracking using the patient’s glucose meter, blood pressure monitor and weight scale showed clinicians that the patient’s glucose level spiked at the same time every night. The patient revealed that he usually ate popcorn at that time but didn’t record it because he thought it was healthy.
READ MORE: 5 key considerations for effective remote patient monitoring.
“In the first 30 days, his A1C dropped by a point. It was the first time he had noticed that a behavior chance could change health, and this systematically changed his health, with his A1C level eventually dropping below 6,” said Schiller. “The patient isn’t a different person, and the healthcare system isn’t a different healthcare system. Data helped provide insight into the patient’s life and led to a conversation about what was happening, not what should be happening. Data works well for people, and it’s the way people want to receive healthcare.”
Nixon, co-founder and managing partner of healthcare innovation firm Nixon Gwilt Law, pointed out that in one program, asthma patients use a peak flow meter to measure how well air was moving in and out of their lungs before and after taking their medication.
“The readings are much better when taking their medication. Before, the patients didn’t have a good sense of what the medication was doing for them. This knowledge is a key part of adherence,” she said.